When you’re trying for a baby, it’s important to know if you’re not ovulating (anovulation) so you can get the right treatment. Find out the potential causes and how to spot the signs with advice from a Flo expert.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Did I ovulate? Everything you need to know about anovulation

Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
When you’re trying to get pregnant, ovulation is the big moment in your cycle. It is, after all, when one of your ovaries releases an egg in the hope of being fertilized by sperm. Any worries that you might not be ovulating every cycle can be stressful. This is especially true since signs of ovulation can be subtle, so it might not be immediately obvious that your ovary isn’t releasing an egg. This is what doctors call anovulation — and the good news is it’s more treatable than you might realize. Here’s the lowdown on anovulation, including signs to look for and how your doctor can help.
Key takeaways
- Anovulation happens when there is an imbalance in the hormones needed for your body to mature and release an egg. Several things can cause these hormonal imbalances, from conditions like polycystic ovary syndrome (PCOS) to lifestyle factors like stress.
- The first sign of anovulation is often irregular periods, which can vary in length, are unusually heavy or light, or are missed altogether. Tracking basal body temperature (BBT) and cervical mucus changes or taking at-home ovulation tests can also reveal signs of anovulation.
- While anovulation can mean it’s harder to get pregnant, it’s highly treatable. So, if you’re worried you might not be ovulating, reach out to your doctor. They’ll help you figure out what’s going on and get you the right treatment if you need it.
What is anovulation?
“Anovulation means that a person is not experiencing ovulation,” says Dr. Jennifer Boyle, obstetrician and gynecologist at Massachusetts General Hospital, US. “This means that their ovaries are not preparing and releasing eggs. If an egg is not released, then pregnancy cannot occur.”Before we dig deeper into why you might not ovulate, here’s a breakdown of what your cycle might look like. A typical menstrual cycle is classed as being 28 days long. However, if yours varies between 21 and 35 days, then — don’t stress — that’s totally normal.
Around the midpoint of your cycle (if you have a typical 28-day cycle), your brain releases gonadotropin-releasing hormone, which stimulates another hormone — follicle-stimulating hormone (FSH) — to make the follicles in your ovaries develop an egg. A surge of luteinizing hormone (LH) then tells one ovary to release a fully mature egg. This is ovulation. Pretty cool, right?
Next, your egg travels down one of your uterine tubes, where it could meet and be fertilized by a sperm. If the fertilized egg successfully embeds in the lining of your uterus (a process known as implantation), you would then be considered to be pregnant. But if your egg doesn’t get fertilized or implant, the hormones estrogen and progesterone drop. This causes the lining of your uterus to shed, and you get your period.
Does anovulation indicate infertility?
So if one of your ovaries doesn’t release an egg, it means you can’t get pregnant in that cycle. This can be a worrying thought. Does it mean anovulation equals infertility? “Not necessarily,” says Dr. Boyle. “It’s critical to keep in mind that very few people don’t ovulate at all. Most people who have anovulation or infrequent ovulation will ovulate from time to time.” In fact, occasional anovulation is fairly common, with research suggesting the chances of not ovulating are from 1% to 14.5% per cycle.
Unfortunately, sometimes anovulation happens enough that couples do struggle to get pregnant. A quarter of female infertility cases are caused by ovulatory disorders, which can include infrequent ovulation or anovulation. But, in many cases, the cause of anovulation can be treated.
“Ovulation problems can be treated in lots of different ways and with a high chance of success,” says Dr. Boyle. “I tell patients that when they’re not ovulating, they’re not really in the game yet. When they start to ovulate or get in the game, they may become pregnant.”
So, if you’re worried you may not be ovulating regularly or even at all, try not to panic. The stats are on your side. Before we look at the ways anovulation is diagnosed and treated, let’s explore what causes it and how to spot the signs.
 Over
7.8M
ratings averaging
4.8/5
*
Over
7.8M
ratings averaging
4.8/5
*
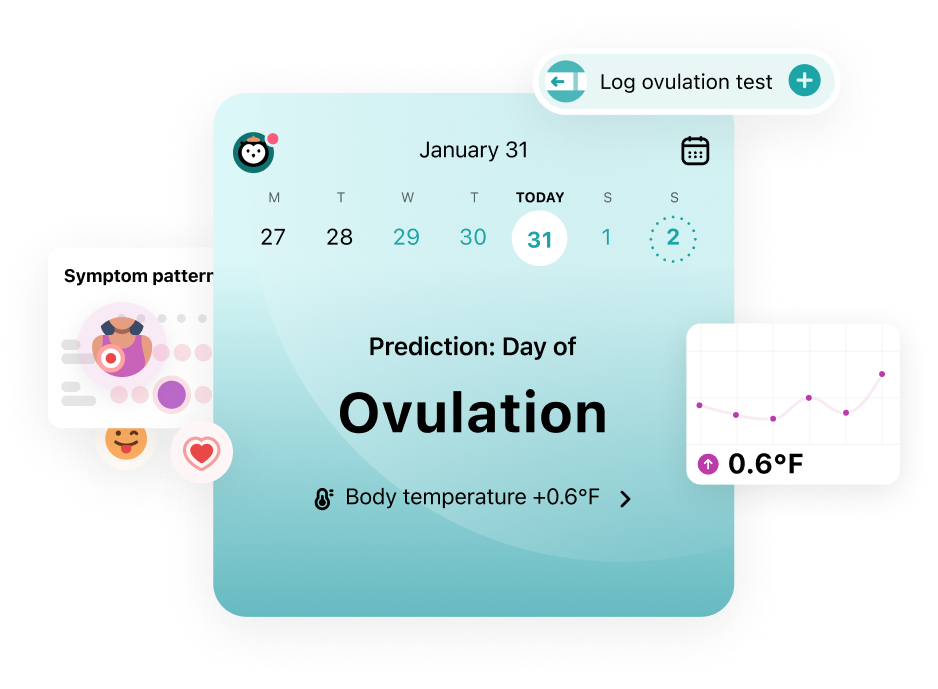
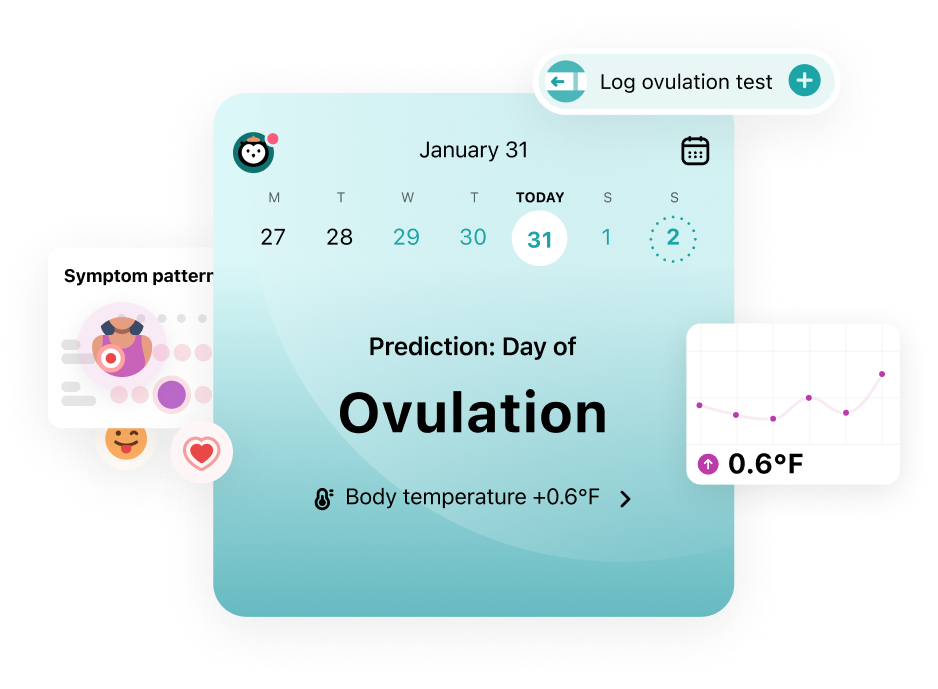
Understand your fertility better with the Flo app
- Learn more about your fertility signals
- Improve ovulation predictions by tracking temperature via Apple Watch
- Log your ovulation test results
 Over
7.8M
ratings averaging
4.8/5
*
Over
7.8M
ratings averaging
4.8/5
*
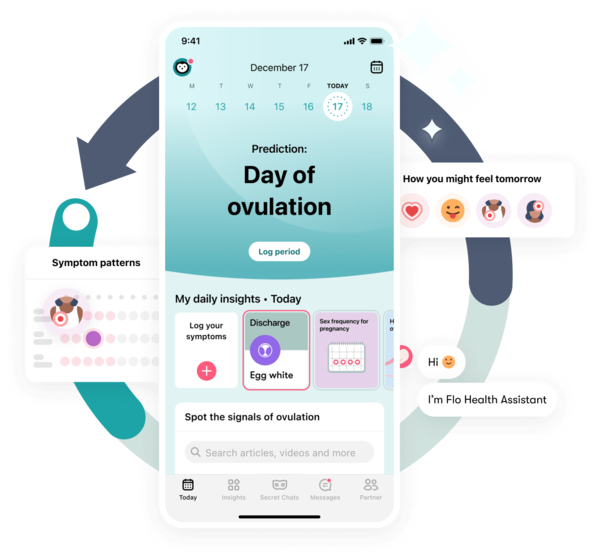
Trying to conceive?
The Flo app can help you better understand your fertility
 Over
7.8M
ratings averaging
4.8/5
*
Over
7.8M
ratings averaging
4.8/5
*
Understand your fertility better with the Flo app
- Learn more about your fertility signals
- Improve ovulation predictions by tracking temperature via Apple Watch
- Log your ovulation test results
“I tell patients that when they’re not ovulating, they’re not really in the game yet. When they start to ovulate or get in the game, they may become pregnant.”
Take a quiz
Find out what you can do with our Health Assistant
What causes anovulation?
There are a number of causes of anovulation, but they all come down to a hormonal imbalance of some kind. This might sound a little scary, but there are lots of different reasons why your hormone levels may change — and some are as simple as lifestyle factors like stress. Here are some of the most common reasons why your hormone levels might affect ovulation.
Polycystic ovary syndrome (PCOS)
You might have heard of the condition PCOS before but not be totally sure what it is. It’s something to get informed about if you think you might not always be ovulating since 70% of anovulation cases are caused by PCOS. It’s pretty common, impacting 8% to 13% of reproductive-aged women worldwide. So, if you find out you have PCOS, you’re far from alone, and the good news is that it’s very treatable.
PCOS causes you to produce a higher-than-normal amount of male sex hormones known as androgens. Everyone produces androgens, but men make more. Often (but not always), PCOS can cause small cysts (fluid-filled sacs) to grow in your ovaries. Having too high androgen levels can stop your eggs from maturing and growing in preparation for ovulation.
The telltale symptoms of PCOS include:
- Heavy, long, or irregular periods
- Missing your period altogether
- Fertility problems and struggling to get pregnant
- Acne or oily skin
- Hair growth on your face and body
- The hair on your head thinning
- Weight gain, especially around your belly
Flo can help you determine if you might have the signs of PCOS. Simply log your cycle symptoms in the app and take our Symptom Checker* questionnaire. You can then take this information to your doctor. They’ll be able to test you for PCOS and figure out your best next step. *Symptom Checker is not available in the UK or EU.
Being over or underweight
Like PCOS, your weight can impact when you ovulate. Weight can be a sensitive subject for some, so try to be gentle with yourself. If you have gained weight over quite a short period of time, then your body may produce too many androgens, which may impact ovulation.
The flip side of this is if you lose weight quickly or exercise excessively, this can cause a delay (or put a pause) on ovulation. You might be curious about how weight loss can impact your cycle. It’s all to do with the parts of your brain that are responsible for producing the hormones FSH and LH. If your weight changes quickly, it can put stress on the parts of your brain that can impact your hormone production, which is so crucial for kicking ovulation into motion.
Stress
We all deal with a certain level of stress in our lives — whether it has to do with work, your home life, or other factors. If you’re feeling very stressed, your body may produce high levels of the hormone cortisol. Among other things, cortisol is responsible for the fight-or-flight response, so it’s there to protect you. However, if you’re overly stressed for a long period, cortisol can disrupt the hormonal balance needed for ovulation. How much stress it takes to have this effect will vary from person to person — it all depends on your personal triggers and how well your body can tolerate it.
Hormonal transitions
Have you just started having periods, or have you started to spot some of the signs associated with perimenopause? The hormonal imbalances during the transitional years of both your teens and perimenopause are normal and can lead to anovulation. It’s totally normal if you find this disruptive or confusing. You might find it helpful to understand what’s going on.
In case you didn’t know, perimenopause is the years leading up to menopause (your final period) when your levels of estrogen start to decrease. During this time, you might notice that your cycles become more irregular. For example, your period may change dates or not arrive at all. It’s worth using a period-tracking app like Flo if you think you might be perimenopausal. You can log your symptoms and keep track of your cycle so that data is ready to share with your doctor.
High levels of prolactin (hyperprolactinemia)
If you’ve had a baby, you might be familiar with prolactin. It’s an important hormone that helps the body to produce milk when you’re breastfeeding. But it is possible to make too much — and that has an impact on your levels of the ovulation hormones FSH and LH, leading to anovulation. This is why if you notice you haven’t ovulated or haven’t had a period in a time when you’re exclusively breastfeeding, it can be chalked up to your hormones.
Breastfeeding isn’t the only reason why your prolactin levels might be high. Certain medications can cause a spike, including some antidepressants or mood stabilizers. Similarly, pituitary gland tumors can be the cause of hyperprolactinemia. If you’re worried that your prolactin levels might have impacted when you ovulate, then it’s a good idea to speak to your doctor.
Thyroid problems
You might think of all the action in your cycle taking place in your uterus, but your thyroid (a gland in your neck) actually plays a key role. It also produces important hormones that keep your body in check. Having either an underactive or overactive thyroid can make your cycle irregular and may mean you don’t ovulate in some cycles. Having an underactive thyroid (also known as hypothyroidism) can lead to a variety of symptoms, including tiredness and weight gain. Meanwhile, having an overactive thyroid (hyperthyroidism) can cause you to lose weight rapidly and have a fast, irregular heartbeat or heart palpitations. If you identify with any of these symptoms, it may be a good idea to reach out to your doctor for a blood test to look at your hormone levels.
Signs of anovulation to look out for
“If you are not ovulating, you will not have a normal menstrual period,” says Dr. Boyle. “Tracking your menstrual cycle and the symptoms that come with it is the best ‘test’ of how your body is doing reproductively.” You can do this using an app like Flo.
However, it’s really important to remember that some variation in your cycle each month is normal and something that many of us will experience. So, how can you spot if your cycle is irregular? Well, irregular periods can look like the following and are always worth speaking to your doctor about.
Irregular in length
Menstrual cycles that are shorter than 21 days or longer than 35 are classed as irregular. If your cycles stay within the normal range but vary in length by seven to nine days — e.g., one cycle lasts 21 days and the next 35 — this is also considered irregular, and you should speak to your doctor. Logging your cycles using an app like Flo can help you figure out your cycle length and have the details ready to share with your health care provider.
Heavy or light
Another possible sign of anovulation is when your period “doesn’t behave like a normal period,” according to Dr. Boyle. She explains: “It might not come with your typical premenstrual warning signs, or it might last longer or be heavier.” So you know what to look out for: Your period should not last for more than seven days or require you to change a tampon or pad less than every two hours.
“On the other hand, anovulatory bleeding can also be lighter than a regular period,” adds Dr. Boyle. “Sometimes, it can just seem like random spotting.” If you notice a dramatic change in how heavy your period is, then it may be worth speaking to your doctor.
A missed or late period
It’s possible to occasionally have a missed or late period due to things like stress. Your cycle is totally unique to you, and while you might spot patterns in it, they don’t always run like clockwork. But if you miss three or more periods in a row, then this is considered irregular and a sign of anovulation to speak to your doctor about.
Your period may be the best place to start, but it isn’t the only clue as to whether you’re ovulating or not. Other signs of anovulatory cycles include:
Irregular basal body temperature (BBT)
Your BBT is your temperature when your body is completely at rest, and it rises very slightly just after ovulation. If you track your BBT using a very sensitive thermometer and it doesn’t follow this pattern, it could be a sign that you’re not ovulating.
No egg white cervical mucus
Just before and during ovulation, your cervical mucus becomes wet and slippery like raw egg whites. Spotting this change is another way to track ovulation. Again, if you don’t notice this, it might be a sign of anovulation. However, the change is slight, so you might struggle to spot this at home.
No positive ovulation test results
Have you tried ovulation predictor kits to help you know when ovulation happens? They work in a similar way to urine pregnancy tests. Before you suspect you’re ovulating, all you need to do is either pee in a cup and dip the test in or pee directly onto the test. If you have used them throughout your cycle but are never getting a positive result, it could mean you’re not ovulating.
It’s important to know that these signs of anovulation are just that: signs, not a diagnosis. Try not to jump to any conclusions until you’ve spoken to your doctor. This may be easier said than done, but they’ll be able to help you figure out what’s going on and work out the best next step. Remember that anovulation is usually easily treated.
How anovulation is diagnosed
If you think you might not be ovulating every cycle, then your doctor will likely ask you about your menstrual cycle history, according to Dr. Boyle. She usually does this by “talking to them about when their last period was and how their periods have been in the past. If someone is having abnormal bleeding that may be due to anovulation, a health care provider will ask questions about what the bleeding is like. How heavy is it? When did it start?”
If this feels very personal, know that your doctor has these conversations every day and is there to help you.

They’ll then look to test for what could be causing anovulation. “This usually starts with a pregnancy test,” she says. “If the pregnancy test is negative, then blood tests will be done to figure out why someone isn’t ovulating.”
She continues: “These generally look to see if there are problems that can prevent ovulation, such as abnormalities in levels of hormones such as thyroid hormone, prolactin, and testosterone. Reproductive hormone levels, such as FSH, are also checked to make sure that anovulation is not due to early menopause.”
Among the tests your doctor might recommend is often a progesterone test. Progesterone is important for supporting your cycle and any pregnancy. As ovulation causes your progesterone levels to rise, the levels in your blood can be a way to confirm whether you have ovulated or not in a given cycle. And if your health care provider suspects PCOS might be causing anovulation, they may want to do a pelvic ultrasound to check if there are any cysts on your ovaries.
Fertility treatment options for people with anovulation
If you are diagnosed with anovulation and want to have a baby, then don’t lose hope. With a little help from a fertility specialist, many couples with ovulation problems go on to get pregnant.
If your periods have become irregular, suggesting that you might not be ovulating every cycle, your doctor may talk to you about your fertility treatment options. Similarly, if you’ve been trying to get pregnant unsuccessfully for one year, or six months if you’re over 35, they may speak to you about fertility treatment. “The treatment options for anovulation will depend on what is causing it,” says Dr. Boyle. “Because there are so many different causes, there are many different treatments.” Here are some of the main ones:
Medications
A fertility specialist can stimulate or regulate ovulation by giving you certain types of medication. For example, clomiphene citrate is a tablet that causes you to produce more FSH and LH and is often the first line of treatment if you are under 39 and don’t have PCOS. Research shows around 75% to 80% of women treated with clomiphene start ovulating, and most of those who become pregnant do so by the fourth cycle. If you have PCOS, doctors may prescribe letrozole, which works in a similar way to clomiphene.
Another type of fertility drug is gonadotropins, which stimulate your ovaries to produce multiple eggs. “Gonadotropins are usually given by injection,” says Dr. Boyle. “These are usually prescribed by a fertility specialist and require intensive monitoring.”
Lifestyle modifications
Depending on why you might not be ovulating every cycle, lifestyle changes can make a big difference. “Stress reduction techniques can help with anovulation due to stress,” says Dr. Boyle. This could mean starting meditation or mindfulness practices. “Extremes of body weight, either under or over, can cause anovulation, so working on exercise and nutrition can help this type of anovulation,” she adds. The best thing to do if you think you might not be ovulating every cycle is to chat with your doctor.
In vitro fertilization (IVF)
IVF can help you get pregnant if you don’t ovulate every cycle, as it removes the need for you to release eggs yourself. Instead, a fertility doctor will prescribe you medication to help stimulate your ovaries to produce a mature follicle. Then, they will collect eggs from your ovaries and fertilize them with sperm in a lab (this may be sperm from your partner or a donor). A fertilized egg will then be placed in your uterus, where it will hopefully implant and continue to develop into a baby. Often, couples will try fertility drugs first before they start IVF.
FAQs
Is anovulation a symptom of PCOS?
Yes, anovulation is a symptom of PCOS. Health care providers will diagnose PCOS if you have at least two of the following three symptoms: irregular periods, signs of excess androgens (e.g., acne or excess facial or body hair), and cysts on your ovaries.
Do you still bleed during an anovulatory cycle?
“It depends,” says Dr. Boyle. “Some people have no bleeding at all when they are not ovulating. However, bleeding can sometimes happen. One of the most common causes of abnormal uterine bleeding is anovulation. What happens is that the ovaries produce estrogen. This stimulates the lining of the uterus to grow and develop [like when you get your period]. It can grow to the point of becoming unstable and start to break down and shed.” This would look like your period.
Do you get cramps during an anovulatory cycle?
“Some people have no cramps when they are not ovulating,” says Dr. Boyle. However, others will still get them. “I’m not sure if we know for sure why this happens, but it is likely due to subtle variations in estrogen levels that occur during the time of anovulation,” she adds.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“About Heavy Menstrual Bleeding.” Centers for Disease Control and Prevention, 15 May 2024, www.cdc.gov/female-blood-disorders/about/heavy-menstrual-bleeding.html.
“Abnormal Uterine Bleeding.” The American College of Obstetricians and Gynecologists, Dec. 2021, www.acog.org/womens-health/faqs/abnormal-uterine-bleeding.
“Anovulation.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/21698-anovulation. Accessed 11 June 2024.
Burkman, Ronald T. “Perimenopause.” Obstetrics and Gynecology Clinics of North America, vol. 29, no. 3, Sep. 2002, pp. xi – xii, https://doi.org/10.1016/S0889-8545(02)00018-9.
“Can Stress Cause You to Skip a Period?” Cleveland Clinic, 18 Sep. 2020, health.clevelandclinic.org/can-stress-cause-you-to-skip-a-period.
“Female Infertility.” Mayo Clinic, 27 Aug. 2021, www.mayoclinic.org/diseases-conditions/female-infertility/diagnosis-treatment/drc-20354313.
Hambridge, H. L., et al. “The Influence of Sporadic Anovulation on Hormone Levels in Ovulatory Cycles.” Human Reproduction, vol. 28, no. 6, June 2013, pp. 1687–94, doi: 10.1093/humrep/det090.
“Hyperthyroidism (Overactive Thyroid).” Mayo Clinic, 30 Nov. 2022, www.mayoclinic.org/diseases-conditions/hyperthyroidism/symptoms-causes/syc-20373659.
“Hypothyroidism (Underactive Thyroid).” Mayo Clinic, 10 Dec. 2022, www.mayoclinic.org/diseases-conditions/hypothyroidism/symptoms-causes/syc-20350284.
“In Vitro Fertilization (IVF).” Mayo Clinic, 1 Sep. 2023, www.mayoclinic.org/tests-procedures/in-vitro-fertilization/about/pac-20384716.
“Irregular Periods.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/14633-abnormal-menstruation-periods. Accessed 11 June 2024.
“Menstrual Cycle.” Cleveland Clinic, my.clevelandclinic.org/health/articles/10132-menstrual-cycle. Accessed 11 June 2024.
“Using Ovulation Tools to Predict Fertility.” Mayo Clinic, 13 June 2023, www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/using-ovulation-kits-to-predict-fertility.
“Polycystic Ovary Syndrome ( PCOS).” Cleveland Clinic, my.clevelandclinic.org/health/diseases/8316-polycystic-ovary-syndrome-pcos. Accessed 11 June 2024.
Pereira-Eshraghi, Camila F., and Patricia P. Vuguin. “Polycystic Ovary Syndrome.” Pediatrics in Review, vol. 45, no. 6, June 2024, pp. 363–65, publications.aap.org/pediatricsinreview/article-abstract/45/6/363/197327/Polycystic-Ovary-Syndrome.
“Polycystic Ovary Syndrome (PCOS).” Johns Hopkins Medicine, www.hopkinsmedicine.org/health/conditions-and-diseases/polycystic-ovary-syndrome-pcos. Accessed 11 June 2024.
“Postpartum Birth Control.” The American College of Obstetricians and Gynecologists, Apr. 2023, www.acog.org/womens-health/faqs/postpartum-birth-control.
“Progesterone Test.” MedlinePlus, 4 Oct. 2022, medlineplus.gov/lab-tests/progesterone-test.
Rebar, Robert W. “Ovulatory Dysfunction.” MSD Manual Professional Edition, Feb. 2024, www.msdmanuals.com/en-gb/professional/gynecology-and-obstetrics/infertility-and-recurrent-pregnancy-loss/ovulatory-dysfunction.
Tadokoro, N., et al. “Cumulative Pregnancy Rates in Couples with Anovulatory Infertility Compared with Unexplained Infertility in an Ovulation Induction Programme.” Human Reproduction, vol. 12, no. 9, Sep. 1997, pp. 1939–44, DOI:10.1093/humrep/12.9.1939.
Taitson, Paulo Franco, et al. “Treating Male Infertility.” JBRA Assisted Reproduction, vol. 17, no. 6, Nov.–Dec.. 2013, pp. 351–52, www.jbra.com.br/media/trab/arq_125.
History of updates
Current version (20 June 2024)
Published (04 October 2018)
In this article
Get your personal guide to fertility
-
Learn how to read your body's ovulation signals
-
Find daily conception tips from our experts
-
Chat with others who are trying to get pregnant




