It’s normal for your periods to change in the run-up to menopause. Here’s why and what you can do about it.
-
Tracking cycle
-
Getting pregnant
-
Pregnancy
-
Help Center
-
Flo for Partners
-
Anonymous Mode
-
Flo app reviews
-
Flo Premium New
-
Secret Chats New
-
Symptom Checker New
-
Your cycle
-
Health 360°
-
Getting pregnant
-
Pregnancy
-
Being a mom
-
LGBTQ+
-
Quizzes
-
Ovulation calculator
-
hCG calculator
-
Pregnancy test calculator
-
Menstrual cycle calculator
-
Period calculator
-
Implantation calculator
-
Pregnancy weeks to months calculator
-
Pregnancy due date calculator
-
IVF and FET due date calculator
-
Due date calculator by ultrasound
-
Medical Affairs
-
Science & Research
-
Pass It On Project New
-
Privacy Portal
-
Press Center
-
Flo Accuracy
-
Careers
-
Contact Us
Why do periods get closer together during perimenopause?


Every piece of content at Flo Health adheres to the highest editorial standards for language, style, and medical accuracy. To learn what we do to deliver the best health and lifestyle insights to you, check out our content review principles.
If your menstrual cycle has been more or less running like clockwork every month since your teens, it can be alarming — and also inconvenient — if your periods suddenly get closer together. Aside from the fact your monthly bleed is usually a good indicator that everything is running smoothly inside, nobody wants to have periods more often, right?
A cycle that lasts anywhere between 21 and 35 days is considered to be a normal length. So if your bleeding pattern does shift occasionally within those limits, it’s usually nothing to worry about. Sometimes you might get two periods in one month, for example, or you might get one a little later than expected. But if you’re anywhere between your late 30s and your 50s and your tracking app shows your periods have been getting closer together lately, it might be a symptom of perimenopause, signaling the start of your journey toward menopause.
Here, obstetrician and gynecologist Dr. Angela Jones, New Jersey, US, shares everything you need to know about your periods getting closer together in your 30s, 40s, and 50s. But if you have any questions or concerns about changes to your bleeds, always reach out to your health care provider for advice.
Key takeaways
- Up to a quarter of women have irregular menstrual cycles. This can mean a number of things, like the time between each period being either shorter or longer than average.
- A change in your periods is often one of the first symptoms of perimenopause.
- Fluctuating hormone levels are the reason why perimenopause can cause unpredictable bleeding patterns, such as your periods getting closer together.
- Some birth control pills can regulate your periods in the early stages of perimenopause and may also help to dial down some symptoms you’ve got. Your doctor will be able to help you decide if this could work for you.
- Hormone therapy (or HT, previously known as hormone replacement therapy or HRT) isn’t usually offered for irregular cycles alone, but if you have other perimenopause symptoms like hot flashes, then it may help. Again, chat with your doctor to figure out what treatment could be right for you.
Is it normal for periods to be closer together during perimenopause?
While no two people have the exact same symptoms, irregular periods can be a sign of perimenopause. So yes — it’s pretty common for your periods to get closer together during this time. But that’s not the only way they can change.
“Periods can do any number of things in perimenopause,” says Dr. Jones. “They can get closer together, further apart, can skip months at a time, and can be characterized by spotting in between,” she explains. “They can [also] be heavy or light, [and] the blood can be light, dark, or brown in color.” In short, any disruption to your periods during this phase of life could well be due to perimenopause.
You’ve probably heard of the term menopause before, so what’s perimenopause? The two are actually separate things. Perimenopause is what we call the years leading up to menopause (the name given to your final period). This can begin anywhere between your late 30s and 50s but most often happens in your 40s. It can take between four and eight years before your periods stop altogether — everyone’s different — but on average, perimenopause lasts about four years.
When you haven’t had a period for 12 months, you’re classed as having gone through menopause (this usually happens between the ages of 45 and 55). From then on, you are postmenopausal.
You might be more familiar with other signs of perimenopause, such as hot flashes, night sweats, and mood swings. Like these, changes to your cycle during the run-up to menopause can generally be due to your hormone levels changing. “Your periods get closer together or further apart due to the fact that the ovaries are starting to wax and wane in their function,” explains Dr. Jones. This means the amount of hormones being produced by the ovaries also becomes quite unpredictable, which is what messes with your bleeding patterns.
It can be hard to keep track of irregular periods and other symptoms when you’re going through perimenopause, and that’s where a cycle-tracking app like Flo can help. In the app, you can log symptoms like brain fog and vaginal dryness alongside tracking your periods. Premium subscribers even get a cycle report each month to help you understand your body better.
What else causes irregular periods?
Your periods might end up a little inconsistent for reasons other than perimenopause, so it’s always worth getting checked out by your health care provider to make sure you know what’s behind it. You may assume you’ve had two periods in one month, for example, but the extra bleeding may instead have been caused by a health issue, including:
- Polyps: Uterine polyps are small growths found inside your uterus that can cause bleeding. They’re not usually serious, but your doctor will always want to confirm the cause of any irregular bleeding, so make sure to book an appointment to get checked out.
- Fibroids: Uterine fibroids are growths in your uterus that can cause changes to your bleeding patterns. Not all fibroids will require treatment, but your doctor will be able to advise you on the best option for you if you have them.
- Infections: Some sexually transmitted infections (STIs) can cause vaginal bleeding as a symptom. If you’ve had unprotected sex recently and are worried you may have an STI, go and get a test. If it does turn out to be an STI, there’s nothing to be embarrassed about — health care providers will have seen plenty of other cases like yours before.
- Endometrial hyperplasia: Thickening of your uterine lining can occur at perimenopause, leading to abnormal periods.
- Adenomyosis: This is a condition where the lining of the uterus begins growing into its muscular wall, and it can cause heavy bleeding outside of your regular cycle.
- Cancer: Some cancers, such as cervical cancer, have symptoms that include bleeding between periods or after menopause, but rest assured, this is rare.
Whatever the cause of your irregular bleeding — whether it’s perimenopause, one of the medical conditions listed above, or anything else — your doctor will want to get to the bottom of it. So make sure you book an appointment just to be on the safe side.
What to expect from your period during perimenopause
If your periods become closer together or hard to predict, it can be frustrating. It’s nice to be able to plan around your cycle, after all. There’s no fail-safe way to know how your periods might behave at this time, says Dr. Jones, but Flo’s clever technology may be able to help you detect some patterns in your cycle and be better prepared. Plus, it’s worth remembering that perimenopause is an important life stage that all women and people with periods go through, and there are plenty of treatment options available if you’re finding the symptoms tricky to manage.

Take a quiz
Find out what you can do with our Health Assistant
As you progress through perimenopause, you might experience any number of the following changes to your menstrual cycle:
- Heavier periods: Your flow may become heavier over time, explains Dr. Jones, “The period may be heavier as the uterine lining has had an opportunity to build up over months,” she says. If bleeding is unusually heavy (for example, if you’re repeatedly soaking through your pad or tampon within an hour), always be sure to consult your doctor.
- Lighter periods: On the other end of the scale, a lot of women experience reduced blood flow or spotting for up to a year before their periods stop completely. “Incomplete shedding of the lining can lead to spotting in between periods or lighter periods,” adds Dr. Jones.
- Skipped periods: Your ovaries may not release an egg (ovulate) every cycle during perimenopause, leading to a missed period. This is often normal. Keep in mind, though, that you’re still fertile. So, if you’re having unprotected sex and you’ve missed your period, consider taking a pregnancy test.
- Longer or shorter periods: If your period previously lasted for four days, but now it’s two or six days, for example, this is normal. You might even experience a random combination of both shorter and longer cycles and periods during perimenopause. Again, it’s all due to the up-and-down hormone levels.
Other symptoms of perimenopause
Everyone’s experience of perimenopause is different. Some people find it difficult to manage tricky symptoms, such as heavy or irregular periods, while others don’t.
Symptoms vary, but most people experience at least one of the following at some point during perimenopause:
- Irregular or missed periods or periods that are heavier or lighter than usual
- Hot flashes that feel like sudden, uncomfortable waves of heat and may come with heart palpitations and dizziness
- Problems falling or staying asleep, often as a result of hot flashes
- Vaginal dryness and discomfort during sex
- Reduced sex drive
- Brain fog that might feel like a lack of focus, poor memory, and difficulty concentrating
- Mood swings, including low mood, irritability, tearfulness, and reduced energy levels
- Joint pain or stiffness
Remember, there are plenty of treatment options for all sorts of perimenopause symptoms — you can read up on them below. Schedule an appointment with your doctor to start discussing which route is best for you.
How to treat perimenopausal symptoms
If perimenopausal symptoms are causing disruption to your life, don’t assume you just have to put up with them. In fact, there are a number of treatment options available to help you feel like yourself again. Some of the main types of perimenopause treatment include:
- Hormone therapy: Taking the hormone estrogen can be an effective treatment for many perimenopause symptoms, including hot flashes, night sweats, and irregular periods. As with many health treatments, there are pros and cons of hormone therapy. Chat with your doctor about it, and they can help you decide whether it’s a good option for you.
- Vaginal estrogen: This is a type of hormone therapy that is used internally to help relieve vaginal dryness, some urinary symptoms, and pain with sex.
- Antidepressants: Some medications usually given for mood disorders have also been found to reduce perimenopause symptoms like hot flashes and night sweats. This could be an option if you don’t want to take HT or if you’ve been advised that you shouldn’t for medical reasons.
- Hormonal contraceptives: Using the combined birth control pill for perimenopause may help to level out your changing hormone levels and could reduce symptoms in the early stages of your transition toward menopause.
- Vaginal moisturizer: Just like the skin on your face, if your vagina feels dry, then regularly applying moisturizer can help to keep it supple, providing relief from vaginal dryness.
- Vaginal lubes: Some people find sex painful thanks to vaginal dryness and less natural lubrication. Applying a pea-sized blob of lube before you get started and during sex can be a great way to stop the discomfort.
- Lifestyle changes: For many people, simple lifestyle changes can help with perimenopause symptoms. “Leading a healthy lifestyle [can help] across the board,” says Dr. Jones. She recommends doing things like “making healthy dietary choices, staying active, getting enough rest, and having outlets to deal with stress.” Are you unsure which foods to include in your diet? Try “adding more protein, fiber, fruits, vegetables, and calcium-rich foods,” she says. Limiting your alcohol and caffeine intake can also help, as “both can exacerbate hot flashes and interfere with getting a good night’s rest.”
- Strength training: Now would also be a good time to focus on strength training to build muscle, explains Dr. Jones. “Decreasing estrogen levels causes a loss in muscle mass,” she says. “Muscle building will help you positively impact your bones, which are also affected by declining estrogen levels.”
- Cognitive behavioral therapy: This talk therapy (also known as CBT) has been shown to be effective in mood-related and sleep-related perimenopause symptoms, as well as hot flashes. Chat with your doctor for more advice on whether to explore this option.
Treatment options differ according to the symptoms you’re experiencing and how severe they are, so reach out to your doctor to discuss your options. They will likely ask you questions about your menstrual cycle, including the length and type of bleeding you experience, so having a record of it on an app like Flo can be useful.
When to see a doctor
If your periods are becoming inconsistent or different, make an appointment with your doctor. “Any change in your bleeding should prompt a visit to your obstetrician and gynecologist (OB-GYN), as perimenopause isn’t the only thing that can cause irregular bleeding/spotting,” advises Dr. Jones. Especially prioritize being seen by a doctor if you’ve got “bleeding that is interfering with your quality of life, specifically, causing you to miss work, or [stopping] you from doing things you enjoy such as hanging out with friends, exercising, etc.” she adds.
If you experience any of the following accompanying symptoms, your health care provider will definitely want to examine you to rule out other causes:
- Heavy periods: Very heavy periods — which Dr. Jones describes as “bleeding through a pad [or tampon] per hour for more than two hours” — accompanied by blood clots larger than the size of a bottle cap should be looked into.
- Fatigue: If you’re struggling with low energy levels, see your doctor: “Bleeding that causes anemia or results in signs such as tiredness or fatigue [may be] concerning,” says Dr. Jones.
- Spotting: Bleeding between periods or after sex isn’t always a cause for concern, but it’s a good idea to get it checked out just in case.
- Periods closer together: While changes to your period are normal, it’s still worth being seen by a doctor if you get two periods in one month or any other variations. “Bleeding that lasts longer than seven days or periods less than 21 days apart are all reasons to see your OB-GYN,” says Dr. Jones.
More FAQs
Why is my menstrual cycle getting shorter in my 30s?
As you approach your late 30s, your periods may become more frequent or get shorter. This is part of perimenopause and your body’s natural transition to menopause.
Can perimenopause cause periods every two weeks?
In theory, yes. It can be common in early perimenopause for the length of time between periods to become longer or shorter, to skip periods entirely, or for your flow to change from light to heavy. In fact, these can be some of the first signs that your estrogen levels are starting to change. If you notice changes like this or anything else to your menstrual cycle, schedule an appointment with your OB-GYN.
What is the average age for perimenopause?
There’s no specific age for perimenopause to start. Perimenopause can begin between your late 30s and 50s but most often starts in your 40s.


Hey, I'm Anique
I started using Flo app to track my period and ovulation because we wanted to have a baby.


The Flo app helped me learn about my body and spot ovulation signs during our conception journey.


I vividly
remember the day
that we switched
Flo into
Pregnancy Mode — it was
such a special
moment.
Real stories, real results
Learn how the Flo app became an amazing cheerleader for us on our conception journey.
References
“Abnormal Uterine Bleeding.” The American College of Obstetricians and Gynecologists, Dec. 2021, www.acog.org/womens-health/faqs/abnormal-uterine-bleeding.
“Adenomyosis.” Mayo Clinic, 6 Apr. 2023, www.mayoclinic.org/diseases-conditions/adenomyosis/symptoms-causes/syc-20369138.
“Combination Birth Control Pills.” Mayo Clinic, 13 Jan. 2023, www.mayoclinic.org/tests-procedures/combination-birth-control-pills/about/pac-20385282.
Delamater, Lara, and Nanette Santoro. “Management of the Perimenopause.” Clinical Obstetrics and Gynecology, vol. 61, no. 3, Sep. 2018, pp. 419–432, doi: 10.1097/GRF.0000000000000389.
“Endometrial Hyperplasia.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/16569-atypical-endometrial-hyperplasia. Accessed 24 June 2024.
Hames, Marty Velasco. “Mayo Clinic Minute: Does Menopause Cause Brain Fog?” Mayo Clinic News Network, 7 June 2023, newsnetwork.mayoclinic.org/discussion/mayo-clinic-minute-does-menopause-cause-brain-fog/.
“Heavy Menstrual Bleeding.” Mayo Clinic, 30 Aug. 2023, www.mayoclinic.org/diseases-conditions/menorrhagia/symptoms-causes/syc-20352829.
“Hormone Therapy for Menopause.” The American College of Obstetricians and Gynecologists, Oct. 2021, www.acog.org/womens-health/faqs/hormone-therapy-for-menopause.
“Hormone Therapy: Is It Right for You?” Mayo Clinic, 6 Dec. 2022, www.mayoclinic.org/diseases-conditions/menopause/in-depth/hormone-therapy/art-20046372.
“Hot Flashes.” Mayo Clinic, 12 Dec. 2023, www.mayoclinic.org/diseases-conditions/hot-flashes/symptoms-causes/syc-20352790.
“Introduction to Menopause.” Johns Hopkins Medicine, www.hopkinsmedicine.org/health/conditions-and-diseases/introduction-to-menopause. Accessed 24 June 2024.
“Irregular Periods.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/14633-abnormal-menstruation-periods. Accessed 31 May 2024.
Krassas, G. E., et al. “Disturbances of Menstruation in Hypothyroidism.” Clinical Endocrinology, vol. 50, no. 5, May 1999, pp. 655–659, doi: 10.1046/j.1365-2265.1999.00719.x.
“Menopause 101: A Primer for the Perimenopausal.” The North American Menopause Society, www.menopause.org/for-women/menopauseflashes/menopause-symptoms-and-treatments/menopause-101-a-primer-for-the-perimenopausal. Accessed 11 June 2024.
“Menopause.” World Health Organization, 17 Oct. 2022, www.who.int/news-room/fact-sheets/detail/menopause.
“Perimenopause.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/21608-perimenopause. Accessed 2 Apr. 2024.
“Perimenopause.” Mayo Clinic, 25 May 2023, www.mayoclinic.org/diseases-conditions/perimenopause/symptoms-causes/syc-20354666.
Potter, N., and N. Panay. “Vaginal Lubricants and Moisturizers: A Review into Use, Efficacy, and Safety.” Climacteric, vol. 24, no. 1, Feb. 2021, pp. 19–24, doi: 10.1080/13697137.2020.1820478.
Silver, Nazanin E. “Mood Changes during Perimenopause Are Real. Here’s What to Know.” The American College of Obstetricians and Gynecologists, Apr. 2023, www.acog.org/womens-health/experts-and-stories/the-latest/mood-changes-during-perimenopause-are-real-heres-what-to-know.
“The 2023 Nonhormone Therapy Position Statement of The North American Menopause Society” Advisory Panel. “The 2023 Nonhormone Therapy Position Statement of The North American Menopause Society.” Menopause, vol. 30, no. 6, June 2023, pp. 573–590, doi: 10.1097/GME.0000000000002200.
“The Menopause Years.” The American College of Obstetricians and Gynecologists, Dec. 2018, www.acog.org/womens-health/faqs/the-menopause-years.
“Uterine Cancer (Endometrial Cancer).” Cleveland Clinic, my.clevelandclinic.org/health/diseases/16409-uterine-cancer. Accessed 24 June 2024.
“Uterine Fibroids.” Cleveland Clinic, my.clevelandclinic.org/health/diseases/9130-uterine-fibroids. Accessed 15 Feb. 2022.
“Uterine Polyps.” Mayo Clinic, 15 Nov. 2022, www.mayoclinic.org/diseases-conditions/uterine-polyps/symptoms-causes/syc-20378709.
“What Are Menstrual Irregularities?” Eunice Kennedy Shriver National Institute of Child Health and Human Development, www.nichd.nih.gov/health/topics/menstruation/conditioninfo/irregularities. Accessed 31 May 2024.
“What Is Cognitive Behavioral Therapy?” American Psychological Association, 2017, www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral.
“What Is Menopause?” National Institute on Aging, www.nia.nih.gov/health/menopause/what-menopause. Accessed 2 Apr. 2024.
“Yes, Weight Loss Can Impact Your Menstrual Cycle.” Cleveland Clinic, Apr. 2023, health.clevelandclinic.org/can-weight-loss-affect-your-period.
History of updates
Current version (26 June 2024)
Published (27 August 2019)
In this article
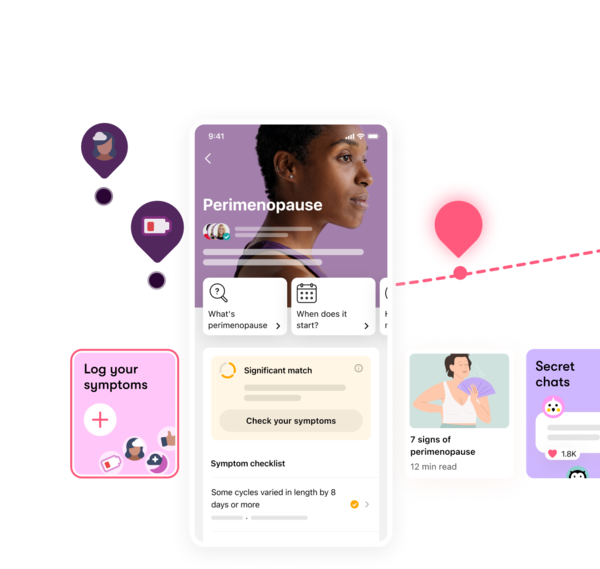
Track your perimenopause journey in the Flo app
-
Log symptoms and get tips to manage them
-
Learn what to expect with expert-led articles and videos
-
Connect with others who can relate to how you're feeling




